An osteochondral lesion of the talus (OLT) is an area of abnormal, damaged cartilage and bone on the top of the talus bone (the lower bone of the ankle joint). This condition is also known as osteochondritis dissecans (OCD) of the talus or a talar osteochondral lesion (OCL). It is often associated with a traumatic injury such as a severe ankle sprain. However, it can also occur from chronic overload due to malalignment or instability of the ankle joint.
OCLs most commonly occur in two areas of the talus :
SYMPTOMS
Many patients with talar OLTs are asymptomatic . OLTs can be an incidental finding on an MRI ordered to assess another problem. However, if the lesion is large enough, or the overlying cartilage is displaced, talar OLTs can be quite symptomatic. These symptoms could include localized ankle pain, as well as discomfort on either the inside (medial talar OLT) or outside (anterolateral talar OLT) of the ankle. The pain is often worse with activities, particularly running, walking and jumping. They may also complain of mechanical symptoms, such as clicking and popping sounds caused by a loose fragment of cartilage and/or bone associated with the OLT.
DAIGNOSIS
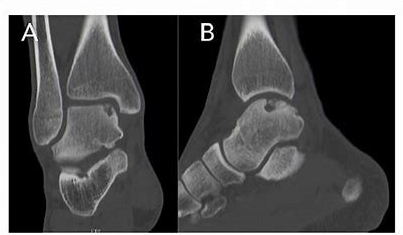
Plain x-rays can be used to help diagnose an osteochondral lesion. Areas of decreased density (i.e., darker areas) seen on the plain x-rays can be indicative of this condition.
The gold standard for diagnosis of talar OLTs is an MRI of the ankle. An MRI of the OLT may show that the cartilage and bone damage is displaced or non-displaced .
Treatment
Non-Operative Treatment Non-operative treatment can be successful for non-displaced talar OLTs, especially if the condition is recognized and treated early, and the lesion is relatively small.

